Introduction
C-sections, or cesarean sections, are not just a medical procedure; they are a significant life event that impacts mothers, babies, and families in various ways. The rise of C-section rates globally is both a testament to medical advancement and a subject of debate among healthcare professionals. While C-sections can be life-saving interventions for both the birther and the baby, they are often performed for reasons that are not medically justified. For instance, the World Health Organization suggests that only 10-15% of all births require a C-section for medical reasons, yet in some countries, the rate is as high as 50%. This discrepancy raises questions about the medical, social, and economic factors driving the high rates.
Understanding what a C-section entails, when it is medically necessary, and the potential risks involved is crucial. This guide aims to delve into the multifaceted nature of C-sections. We will explore medical and non-medical reasons for the procedure, discuss the risks involved, look at emerging trends like “gentle C-sections” that aim to make the experience more humane and emotionally fulfilling for the birther and family and explore the healing process after a C-section. By the end of this guide, you’ll have a comprehensive understanding of C-sections, empowering you to make informed decisions regarding your healthcare.
What is a C-Section?
A Cesarean Section, commonly abbreviated as C-section, is a major abdominal surgical procedure specifically designed to deliver a baby when vaginal delivery is not possible or safe for the birther, the baby, or both. Performed by an obstetrician, the C-section has undergone several refinements and is now often referred to as the Lower Segment Cesarean Section (LSCS).
During the procedure, the birther is generally awake, thanks to spinal anesthesia that numbs the body from the waist down. This ensures the individual remains aware of their surroundings without feeling the pain of the surgery. The surgical process is meticulous and involves multiple steps. An incision is first made horizontally across the lower abdomen. This is followed by cutting through the adipose tissue and then incising the rectus abdominal sheath, a fibrous layer that covers the abdominal muscles. The transverse abdominal muscles are separated to access the peritoneum, a thin membrane covering the internal organs, which is also cut to reach the uterus.
The next step involves making another horizontal incision in the uterus and puncturing the amniotic sac to deliver the baby. Following the baby’s delivery, the placenta is removed. The uterus and other incised layers are then sutured back together using a double suturing technique, which aids in better healing and makes future VBAC attempts more likely.
The surgery itself usually takes around 45 to 60 minutes, but the spinal anesthesia wears off approximately 4 hours post-surgery. Many hospitals encourage the birther to walk to the bathroom to urinate, assisting in preventing post-surgical complications like Deep Vein Thrombosis (DVT).
C-section is the most commonly performed surgery worldwide. Many of the obstetricians are experts and it is generally considered very safe. However, it’s crucial to understand that a C-section is not devoid of risks and potential complications and there are consequences of the surgery that need to be taken into account when offering it to the birther.
It is often considered a last resort when other forms of delivery present greater risks. But there are numerous instances where C-sections are performed without medical indications, raising ethical and healthcare concerns. By understanding what a C-section truly involves—medically, physically, and emotionally—one can make a more informed decision when faced with the various options for childbirth.
Medical Indications for a C-Section
The most frequent medical indication for a C-section is unresolved fetal distress. This is when the baby’s heart rate goes below the range of normal and does not recover despite appropriate clinical management during labor. This indicates that the baby is running out of resources, is unable to withstand the rigors of labor, and needs to be rescued.
The decision to perform a Cesarean section can also be influenced by variety of other medical factors concerning the health of the birther and the baby. Other reasons for C-sections are:
- High, uncontrolled blood pressure in the birther.
- Unexplained bleeding from the vagina could indicate underlying complications like placental abruption.
- Placenta previa or low-lying placenta- where the placenta is covering a part of the cervix or the whole cervix.
- If the baby is in a transverse position, it could obstruct vaginal birth.
- Cephalo pelvic disproportion (CPD) – if the birther’s pelvis and the baby are not the right fit, the baby cannot be born vaginally. CPD is extremely rare but is often overdiagnosed.
- Cord prolapse – when the umbilical cord slips out of the cervix or vagina or both before the baby is born. The cord is the baby’s lifeline and when it washes out before the head, it gets compressed between the birther’s pelvis and the baby’s head, depriving the baby of oxygen
- Twins which share the same amniotic sac and placenta (Monochornic and Monoamniotic) require a C-section
- Uterine rupture- When the uterus gives way and separates before the birth of the baby, a c-section can be a life-saving procedure for both the birther and the baby.
- Failure to progress or labor dystocia- This birth complication is often tricky to diagnose and is often overdiagnosed. This may happen more in cases where labor is induced or artificially started.
- Failed induction- Starting labor artificially for medical or non-medical reasons can increase the risk of c-sections by up to 50%. Typically induction usually indicates a cascading effect of interventions, one leading to another. While in some cases it is necessary to ensure the safety and well-being of the birther and the baby, there is a tendency to overuse this intervention. Please note that 6-8 hours of induction does not amount to a failed induction as is the case in some hospitals in the world. Induction usually takes time as the body and the baby are often not ready for labor, so more coaxing and time are needed.
Most of the above-mentioned complications are quite rare. According to WHO, 10-15% of the birthers may need a c-section. This means at least 85% of birthers can give birth vaginally. How is it then in many countries the c-section rates are much higher?
Non-Evidence Based Reasons for a C-Section
Cesarean sections are becoming more common, yet not always for medically justified reasons. While some C-sections are medically necessary, many are performed based on unsubstantiated or outdated beliefs.
- Myth of the Overdue Baby: The notion that babies must be born on or before their estimated due date (EDD) often leads to unnecessary C-sections. In reality, only 5% of babies arrive on their EDD. A whopping 60% of babies are born 10-15 days after the due date. As long as the mother and the baby are doing fine in terms of their clinical assessment, waiting for labor to start is the right approach.
- Big Baby Fallacy: The diagnosis of macrosomia (or “big baby syndrome”) is often cited as a reason for C-section. Without a trial of labour, there is no conclusive way of saying that the baby cannot be born vaginally. GDM (Gestational Diabetes) birthers typically have a higher rate of macrosomic babies.
- Misconceptions About Meconium: The presence of meconium-stained amniotic fluid is often inaccurately linked to fetal distress, leading to unnecessary C-sections. When babies pass meconium, the first poop, either before labor or during labor & birth, many care providers will recommend a c-section to prevent MAS or meconium aspiration syndrome. Around 15-20% of term babies (37-40 weeks) and 30-40% of post-term babies (40 weeks onwards) pass meconium during labor which may or may not be related to fetal distress. There is no evidence to corroborate that the presence of meconium causes fetal distress. Of all of these babies 98-97% of the babies are born normally and are healthy. The remaining 3-5% of babies develop MAS where the meconium is aspirated or inhaled into the lower lobes of the lungs causing respiratory distress. Of these babies, 97-98% recover with treatment. There is a 0.06% chance of the baby dying, but these babies usually have other health issues like prematurity, genetic issues, or heart conditions. So in and of itself, meconium-stained amniotic fluid is not a reason for c-section when there are no other health risks present for the baby.
- Nuchal Cord Misunderstanding: A cord wrapped around the baby’s neck (nuchal cord) is often misinterpreted as a reason for a C-section, even in the absence of fetal distress. While babies in the last few weeks of pregnancy practice breathing, they breathe in amniotic fluid. The oxygen is supplied to the baby via the umbilical cord and the placenta. The cord is made up of a gelatinous substance called Wharton’s jelly and three blood vessels. The cord can get wrapped around the baby’s neck or other parts of the body as the baby moves in utero. As long as there is no fetal distress, this reason alone is not in and of itself a complication warranting a C-section
- Breach baby: about 3-4% of babies are buttocks down or head up during the last few weeks of the pregnancy and during labor. Breech birth is a variation of normal and these babies can often be born vaginally. However many of these cases end up in c-sections. There is a growing body of doctors and midwives who are trained, skilled, and experienced in breech births.
- Malpositioned baby: Sometimes babies get into a position where it takes more time for the baby to fit into the pelvis to be born. There are tools to help resolve this that can be considered before going in for a C-section.
- Profit and Convenience: Sometimes, the decision for a C-section is based more on hospital logistics or financial incentives than on the well-being of the birther and baby.
Scheduled vs. Emergency C-Sections
Most c-sections are performed due to complications in labor (listed above) and are referred to as emergency c-sections. Scheduled c-sections are when there are conditions where having surgery is the only option for the birther and the baby. E.g. placenta previa, MAMC twins, and transverse lie.
Often the surgery is scheduled for future pregnancies following a c-section. However, having a VBAC- vaginal birth after a c-section is a possibility that needs to be explored.
Risks of C-Sections
A major abdominal surgery comes with its own risks for the birther and the baby.
Possible risks of c-section include
Postoperative Infection: Risk of infection in the surgical wound or the uterus.
Persistent pain after the operation, requiring medication management.
Hemorrhage: Excessive blood loss during surgery, sometimes necessitating transfusion.
Blood Clots: Potential development of blood clots post-surgery, increasing risk of thromboembolic events.
Low-lying Placenta: Risk of low-lying placenta in subsequent pregnancies.
Placenta Accreta: Placenta could grow too deeply into the uterine wall, complicating future pregnancies.
Uterine Rupture: The scar from the previous C-section might rupture in a future pregnancy.
Adhesions to Urinary Bladder: With multiple c-sections, there’s a risk that the healing wound on the uterus may attach to the bladder, causing urination issues or complications in repeat C-sections.
Chronic Back Pain: Long-term back pain as a potential side effect of the surgery.
Risks for the baby include
Risk of Injury to the Baby: Increased risk of injury to the baby during the surgical procedure.
Hematoma or Clots: Potential for the baby to develop blood clots or hematoma during surgery.
Microbiome Exposure: The baby misses out on exposure to vaginal flora, which could be important for long-term health.
Breathing Difficulties: Newborns may experience transient tachypnea, a temporary breathing problem.
Increased risk for Asthma: Increased likelihood of developing asthma.
Obesity: Higher risk of obesity later in life.
Gentle C-Sections
The traditional approach to C-sections has often been a clinical, detached experience for birthers, featuring limited interaction with the medical team, secured arms, and an obstructive screen that prevents visual engagement during the surgery. However, a rising trend called “gentle C-sections” is transforming the experience into a more humane and inclusive one.
In a gentle C-section, not only are your hands left unsecured, but the obstructive screen is also removed, offering you a direct view and participation in your own birthing process. The medical team walks you through each step, and you even have the option to wear sterile gloves to assist in birthing your baby. One of the most noteworthy aspects is the practice of delayed cord clamping. Unless there’s a medical issue, the baby is immediately placed on your chest for skin-to-skin contact, and you and your partner get to decide when to clamp and cut the umbilical cord. This approach not only promotes bonding but can also facilitate immediate breastfeeding. Some providers even swab the baby’s face with the birther’s vaginal mucus to mimic exposure to the vaginal microbiome, enhancing the baby’s microbial inheritance.
This inclusive approach benefits the whole family, making the birth more participatory and emotionally fulfilling.
Healing After a C-Section
Undergoing a C-section is not just a surgical event; it’s a significant life experience that leaves lasting impacts on both the birther and the baby. The journey of recovery can be arduous and layered, encompassing not just the physical healing but also the emotional and psychological well-being of the birther.
The First Few Weeks
A c-section can have many a ripple effect on the birther and on the baby. Irrespective of the mode of birth, it is hard work that your body has done. So do ensure that you get ample rest for at least the first 2 weeks to initiate the healing process.
Immediate post-surgery care is crucial for avoiding complications. You will be asked to walk to the bathroom to pee after 4-8 hours post-surgery. This helps your blood to circulate through your body after having the anesthesia and prevents any clots from forming. Care should be taken that the stitches remain dry and clean, free of any infection. Signs of infection include pus, swelling, redness, pain, fever, chills, and whole-body aches. Usually, a round of antibiotics is prescribed as a preventative measure. Painkillers and stool softeners are commonly provided to ease discomfort.
Breastfeeding poses unique challenges post a C-section. Positions like side-lying or laid-back are recommended to reduce pressure on the incision area and to ensure that your baby doesn’t accidentally kick your lower abdomen. Reach out for help from the hospital staff to get breastfeeding going.
If your baby is premature or has any health issues, then they may have to be admitted to the Neonatal ICU (NICU) for treatment and monitoring. If there is separation, then ask the staff to help you express your milk to feed the baby.
Emotional Recovery
The emotional aspects following a C-section can be complex. Many times, the birther has unresolved feelings and thoughts after the surgery. Feelings of failure or inadequacy are not uncommon, especially if the surgery was unexpected or unexplained and the birther’s questions before the surgery were unanswered or the need for surgery was not explained. Birth preparation during pregnancy can go a long way in preventing this situation from occurring.
Postpartum is a very vulnerable phase and to top it if you have had surgery it can become an even more difficult phase! Professional emotional support can be invaluable during this time. Do not hesitate to reach out to your birth team, or your care providers if you are having mixed or negative feelings about your experience. Processing your birth with a qualified care provider or a therapist can help in the first few weeks after birth.
The First Few Months
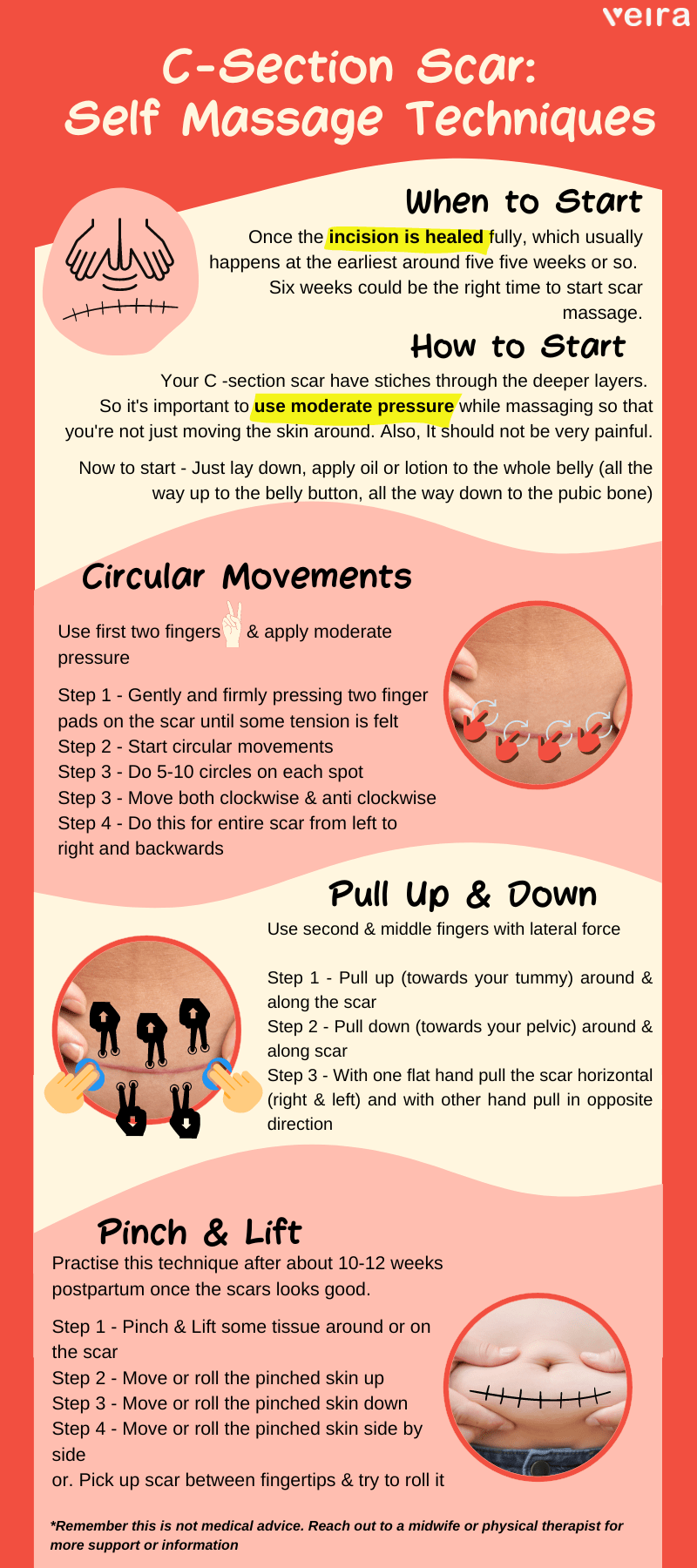
The first couple of weeks are usually spent mostly resting in bed. As weeks pass, the stitches get absorbed by the body, but internal healing may take longer. Around the 6-8 week mark, gentle exercises can be introduced. C-section scar massages can help break down any adhesions and facilitate faster healing. This is also a very warm way of sending love to the part of your body that enabled you to have your little one in your arms. A belly binder can be worn after the first 4-5 days for up to 40 days to support muscle healing. Continued emotional support is essential for a well-rounded recovery.
Check Out Our Infographic on C- Section Self-Massage Techniques Below-
Conclusion
How VeiraLife Can Help You?
Comprehensive Guides: From pre-op to post-op care, our detailed articles, checklists, and recovery timelines will leave no stone unturned.
Expert Advice: Speak to our certified healthcare professionals about your unique circumstances and concerns, whether they are medical or emotional.
Holistic Wellness: Alongside medical advice, our platform offers mental health resources to help you process the emotional aspects of a C-section.
If you’re feeling overwhelmed or need specific guidance, Veira Life is here to help. Connect with us today and empower yourself through every step of your journey.
FAQs
The night before your C-section:
- Follow your doctor’s instructions including any fasting guidelines.
- Pack essentials.
- Confirm transportation & childcare.
- Take a Pre-op shower to help minimize risk of infection.
- Get a good night’s sleep.
- Discuss concerns with your partner and healthcare provider.
These simple preparations can help set the stage for a smoother surgical experience.
Recovery from a C-section is different from a vaginal delivery and generally takes longer. While the doctor may advise bed rest on the first day, movement is usually encouraged soon after to aid in healing. However, it’s important to note that it can take up to 6 weeks for the incision to fully heal. Always consult your healthcare provider for personalized guidance on when it’s safe for you to sit and engage in other activities post-surgery.
Generally, it is advisable to start walking within 24 hours after a C-section surgery. Walking can help alleviate gas pains, promote bowel movement, and reduce the risk of blood clots. However, it’s crucial to follow your healthcare provider’s guidance for a safe recovery. Gentle exercises like deep breathing can be attempted a few days post-surgery; inhale deeply 2-3 times every half-hour. Always consult your doctor for personalized advice.
After a C-section, it’s crucial to take precautions to ensure proper healing. Avoid taking baths until your incision is fully healed and you’ve stopped bleeding. Stay away from public pools and hot tubs to minimize infection risk. Additionally, refrain from lifting anything heavier than your baby to prevent strain on your incision. Always consult your healthcare provider for personalized advice.
After a C-section, it’s recommended to sleep on your side, specifically your left side if possible. Sleeping on your left side is known to increase blood flow to vital organs, which can aid in the healing process. This position is also the most commonly preferred, offering you comfort and relaxation during recovery. However, the best sleeping position can vary from person to person, and it’s important to consult your healthcare provider for personalized advice

Author Bio
Chetana is a skilled and passionate Childbirth Educator trained in the Lamaze philosophy of childbirth preparation. She is also a Lactation Educator-Counselor and practicing midwife. She has developed a holistic childbirth preparation course which she has delivered to hundreds of families and has founded a highly rated natural birth center in Bangalore, India. She has over 11 years of experience supporting families through their journey and transition into parenthood.